
POE in Action: Value Across the Facility Lifecycle
Although POE is a commonplace term in the design and construction industry, its definition and practice have been highly inconsistent across firms and owner organizations. At HDR, we maintain a bank of consistent, validated facility evaluation measures and tools. In any specific evaluation, we draw from that library of measures, as is relevant for the particular evaluation timing and purpose. We believe that more standardization and validation of measures across the industry should be a shared goal.
Somewhat ironically, despite varying evaluation foci, measures and implementation practices across the industry, there does seem to be consensus around the idea that POE should occur in a specific time range (e.g., 12 to 24 months) after a new or renovated facility is occupied. Indeed, we have found without fail that POEs conducted in new facilities during this post-occupancy time period reveal issues that can and should be addressed, and that results can inform future designs. Although design issues have emerged in these evaluations, most often the solutions have entailed fairly minor operational changes or staff training that the organization can easily implement. The cost of an organization not knowing about and not addressing such issues is far higher than the cost of conducting a POE.
A shortcoming of this conception of POE timing is that it tethers facility evaluation to recently-completed architectural projects. In fact, facility evaluation can be fruitfully appIied at many points in the facility lifecycle, and does not have to be at all related to a specific architectural project. (see diagram)
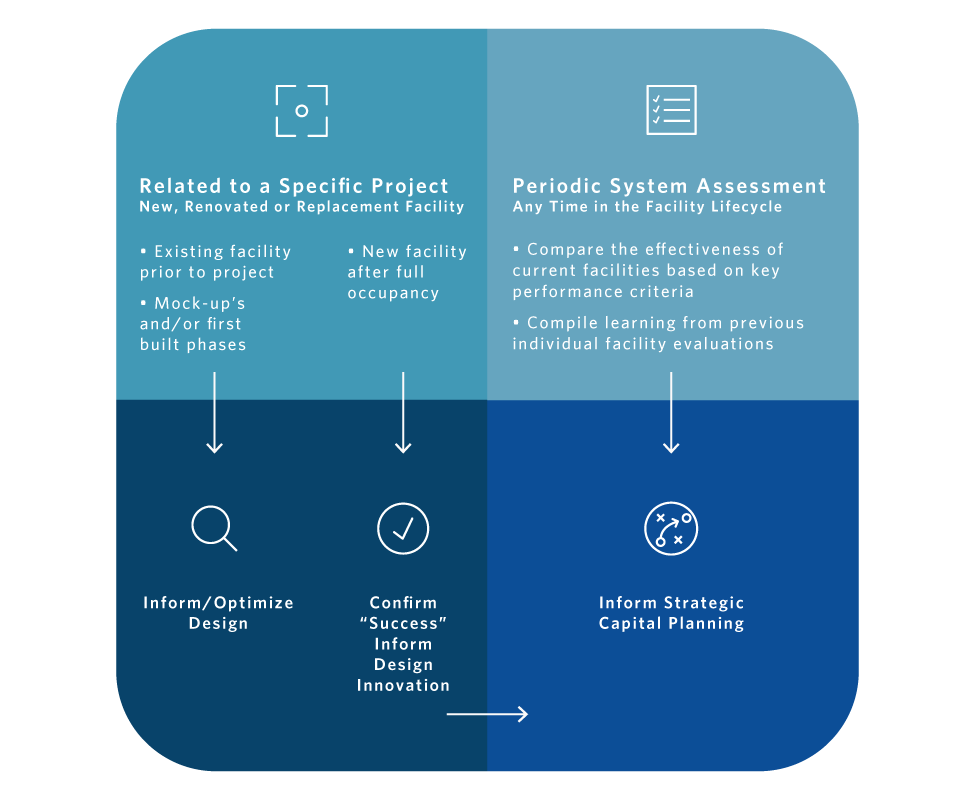
Here we highlight two examples of recent POEs that illustrate the value of facility evaluation at different points in the facility lifecycle. In the first example, evaluation was conducted during construction to inform Phase 2 of an inpatient unit design. The second example highlights how facility evaluation can enable an organization to understand the strengths and weaknesses of its facility stock, contributing to best decision-making in a master planning process.
Advocate Christ Medical Center
Advocate Christ Medical Center is part of Advocate Health Care, one of the nation’s leading health care networks. A not-for-profit, 749-bed, premier teaching institution with more than 1,300 affiliated physicians, the medical center is one of the major referral hospitals in the Midwest for a number of specialties. Following the completion of Phase 1 construction in the renovation of the neonatal intensive care unit (NICU) at Advocate Christ Medical Center in Oak Lawn, Illinois, HDR conducted a facility evaluation. Results from this evaluation are usefully informing the Phase 2 project design.
Evaluation Background
Driven by a goal to maximize family satisfaction, this Advocate project includes a horizontal expansion to double the existing NICU’s square footage. Phase 1 of the project included sixteen single patient rooms, replacing the previous open bay. The unit is now configured in a racetrack layout, with smaller “neighborhoods” located off the main flow path. Each neighborhood consists of eight to 12 mirrored-layout patient rooms with adjacent tandem decentralized “cockpit” nursing stations. Two neighborhoods were completed in Phase 1.
The new NICU environment features four zones to address patient, family and staff space requirements:
- Charting Alcoves
- Caregiver Area
- Patient Area
- Family Area
The facility evaluation included feedback from 103 members of the unit’s nursing staff on the following elements of the new NICU design:
- Aesthetics
- Safety and Security
- Family Centered Care
- Collaboration
Key Findings
Satisfaction with the Phase 1 Design:
- Most respondents expressed satisfaction with the aesthetic design of the new NICU. An overwhelming majority approved of the new floor color and pattern, as well as wall colors and artwork.
- The majority of nursing staff expressed satisfaction with the equipment provided in the NICU, and felt that no equipment was missing.
Mixed Results:
- There was a significant age-based difference in respondents’ opinions as to whether the new single-patient room design enhances patient care. Only 36% of staff over 35 years of age believed that the private room NICU design enhances patient care, while 66% of younger staff said that the design does enhance care (Chi-square test, p=0.01).
- A few staff members noted that anticipated future patient acuity trends may increase work demands on staff to effectively monitor high-acuity patients in separate rooms.
Issues to Address
The facility evaluation identified several areas of staff concern that need to be addressed operationally and/or in the Phase 2 design.
- Nursing staff reported safety concerns in the Phase 1 unit due to perceived inadequate visibility to monitor patients with the single room layout and frosted glass on patient room doors.
- An overwhelming majority (92%) of nursing staff wanted to change the counter height in Charting Alcoves to sitting height, with ergonomics and ability to have feet on the floor while working as the most-stated reason.
- A majority of respondents (78%) were dissatisfied with the tandem Charting Alcove design, and considered it too small to accommodate two working nurses.
- In the Caregiver Area, staff were dissatisfied with the locations of hand sanitizer dispensers, gloves and the proximity of soap dispensers and paper towels to the sinks.
- Nursing staff also expressed dissatisfaction with the amount of storage, cabinet height that was difficult to reach, and the number, types and locations of linen hampers and waste receptacles in the Patient Area.
- In the Family Area, staff noted that the chairs did not offer enough comfort or functionality for “kangaroo care.”
- Feedback also revealed that televisions in the patient rooms, programmed to access health education content only, were generating frustration among family members trying to access standard television content. For this reason, many suggested that it would be preferable to remove the TVs from patient rooms altogether.
The phased renovation approach has allowed an opportunity to gain valuable user feedback to improve next-phase design.
Changes approved in Phase 2 plans include the following:
- Single seat Charting Alcoves
- More proximal locations of glove and hand sanitizer dispensers
- Lower height storage cabinets
- Larger storage rooms
Phase 2 construction currently awaits permits and will include an additional 45 patient rooms, including two twins rooms, within an additional 5 neighborhoods. Phase 2 will also include amenities such as a staff lounge, respite room and consultation room. Once Phase 2 is complete, the new NICU will comprise 61 patient rooms.
Ann & Robert H. Lurie Children's Hospital
For more than 130 years, Ann and Robert H. Lurie Children’s Hospital has worked to advance the health and well-being of all children. Poised for significant growth, the academic-affiliated health system faces questions as to how its current and potential future facilities can best be located and structured to enable growth while reinforcing a consistent and positive branded experience. As one component of the master planning process, HDR conducted facility evaluations to assess the functionality and occupant experience at multiple Lurie Children’s off-site locations.
Evaluation Background
The purpose of the facility evaluation effort was to inform the organization of the relative employee-perceived strengths and weaknesses of its off-site facilities.
In this case, sixteen select measures within Building, Work Space and Work Outcome domains were scored on a validated bimodal scale (converted to a -10 to 10 range for ease of interpretation and visualization in reporting). Scores were compared both across and within facilities to identify relative strengths and weaknesses in the facility stock. The results are available to the organization via an integrated and interactive dashboard that also includes other site data and area populations and trends.
The included domains and measures were as follows:
- Building Measures
- Building location
- Workplace design
- Space adequacy
- Patient/family accommodations
- Privacy
- Staff amenities
- Wayfinding
- Nature and views
- Outside appearance
- Work Space Measures
- Acoustical environment
- Lighting adequacy
- Thermal comfort
- Indoor air quality
- Technology
- Work Outcome Measures
- Collaboration experience
- Collaboration effectiveness
Key Findings & Opportunities
- Among the fifteen off-site locations measured, two scored highest overall, receiving mostly high positive scores across the measures. The organization may do well to emulate these facilities in future expansion.
- Of the environmental measures, building location and lighting adequacy had the highest average scores across all sites. Although convenience and desirability of building location, on average, was in the positive range, some facilities scoring lower on location also had other low scores and may represent opportunities for changes in future planning.
- There were some significant response differences based on whether respondents provided direct patient care or not. Direct patient care staff, more often non-patient care staff, indicated that their physical environment supported workflow and efficiency, and that they had adequate space to perform their work.
- Collaboration experience and effectiveness scores were positive at every location, with a notable overall correlation between better work outcomes and higher scoring buildings and work areas, reinforcing the notion that a quality work environment impacts how well work gets done.
- Technology and nature and views measures scored in the negative range on average. These aspects of the facilities may warrant improvement at all or nearly all locations.
Conclusions
These POE applications, one in a single hospital inpatient unit and one across multiple ambulatory care sites in a healthcare system, differed greatly in purpose and content, while using consistent, validated measures to gain useful feedback. The results are supporting organizational goals ranging from optimizing a unit design, to supporting highly informed capital planning decisions.
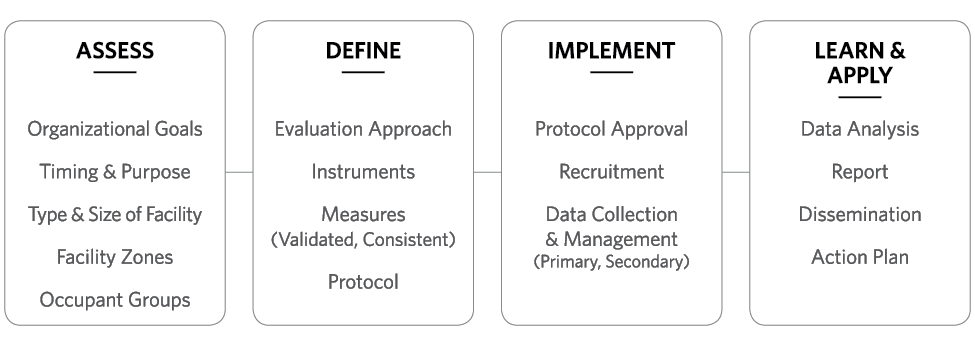
At HDR, POE is not “one size fits all.” While validated, consistent measures are a given, the timing and content of a POE are flexible, depending upon assessment of an organization’s goals, the purpose of the evaluation, and whether and where there is intention to publish results. (see diagram; feel free to design it better) Regardless of the scope in any given case, HDR works with our clients to achieve the turnaround timing needed to support organizational needs and milestones.

