OR Utilization: A Misleading Indicator of Operational Performance
Throughout the last couple of years, improving operational performance has been a leitmotif to all clients with whom I’ve been working. Indeed, executive leadership aims to improve efficiency in order to remain competitive in the market. The idea behind this endless improvement cycle is to retain existing staff and patients, attract new staff and patients, and achieve revenue maximization.
Operational efficiency is measured through quantifiable performance indicators. In the surgery environment, operating room utilization is a widely used metric to inform operational achievement. However, using the “OR utilization” metric is a misleading indicator as it doesn’t inform fully the wellness of an organization’s operational efficiency. And here’s why.
What is “OR Utilization” telling us?
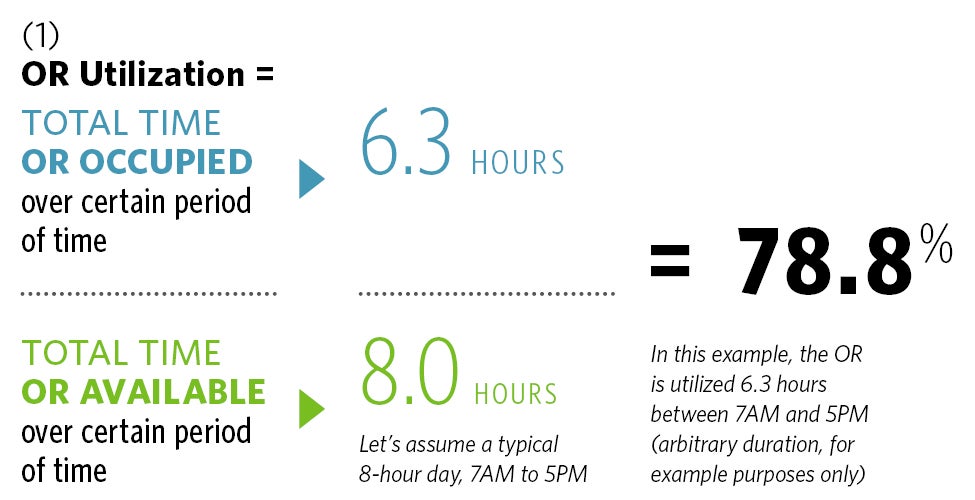
OR utilization indicates the percentage of time an OR is being occupied over a certain period of time. ORs are commonly targeted to be used 75% to 80% of the time.
What is “OR Utilization” not telling us?
OR Utilization as defined above does not depict the inefficiency of operations. Inefficiency can be generated through a poor scheduling process generating significant patient waiting times. For example, a patient (Deborah) is scheduled to have surgery from 2PM to 4PM but the previous case was longer than expected. Deborah is having surgery at 4 PM. Deborah then had to wait two hours before having surgery and the surgical team will still be operating after 5PM.
In this scenario, the OR is occupied at a certain rate from 7AM to 5PM (let’s say, OR Utilization = 75%) but could be running after 5PM as inefficiencies occur throughout the day, such as the delay in Deborah’s surgery. As these inefficiencies occur, patients can end up waiting several hours for an OR to be available. As we all know, patient waiting time and after hours delays negatively impact the patient and staff experience. It’s important to emphasize that looking only at the OR utilization rate doesn’t allow a comprehensive picture of operations efficiency.
Solutions to palliate this issue
Throughout my career at HDR, I have been using an operation-oriented, simulation tool (a more technical term is “discrete event simulation”). Once developed, the simulation model constitutes a virtual environment of a surgery suite, including staff and patients. When the model is running, it’s like watching a video game. The only difference is that patients and staff don’t navigate randomly in the space, but rather follow pre-set and realistic processes.
As every single second passes before your eyes, the simulation tool tracks how long ORs are utilized and when, which will then provide the OR utilization. It also keeps track of patient waiting times and all activities occurring in the ORs after standard hours of operations.
The OR utilization as defined in formula (1) is commonly used in healthcare organizations as the main performance indicator. However, a high OR utilization rate does not necessarily mean “efficient” operations. Depicting only the occupation rate over a certain period of time, the OR utilization does not inform “how efficient” a system is. Patient wait times and the “after hour” delay are meaningful indicators of surgery suite performance.
Considering only OR utilization is similar to only seeing the tip of the iceberg. Incorporating other quantitative metrics like patient waiting time and after hour delays provides a comprehensive understanding of a system's capabilities, and prevents leadership from making decisions based on incomplete information.