Designing With Long-Term Vision: Flexible, Connected and Experience-Focused Outpatient Facilities
Elevating Outpatient Care by Design
Identity deepens the emotional connection between health systems and their communities. Buildings should express commitment to care, respond appropriately to their context and reflect local culture in ways both subtle and expressive. With health systems expanding their patient populations and adding new facilities to bring care closer to home, consistency across a broad range of services is becoming increasingly important.
As strategies, experience expectations, technology and construction evolve, design of outpatient facilities should enhance human experience, support flexibility in care delivery and technology, and embody a health system’s vision.
Strategy First: Both Visionary and Practical
Health systems are increasingly having to do more with less and make tough decisions on how to continue to improve access and growth through outpatient facilities. Aligning health system strategies with design, data and standards can determine a holistic approach, including a path forward for new or remodeled facilities.
Developing a long-term vision requires robust data to help health systems identify shifts in demographics and heath priorities. By coupling design team data with health system data, teams can determine practical paths to achieve long-term vision while meeting short-term goals. A seamless system of care is the aim, informed by big picture trends, technology and innovation shaping utilization and service delivery.
The outpatient center strategy for Advocate Health Care in Chicago has produced more than 30 clinics over the past 10 years. A modular approach coupled with proper population and care needs analysis opens the multiproject endeavor to the evolution of a design language that meets the needs of each community in which it is implemented.
Flexibility Is Paramount: Standardization and Modularity
As populations change, so does a community’s health profile and required service lines. Demographics change, service lines expand and contract, and technology advances, ultimately requiring shifts in space uses and new modes of connection. This, combined with the current costs of construction and high escalation, makes it critically important to think about ways to design flexibility in outpatient environments.
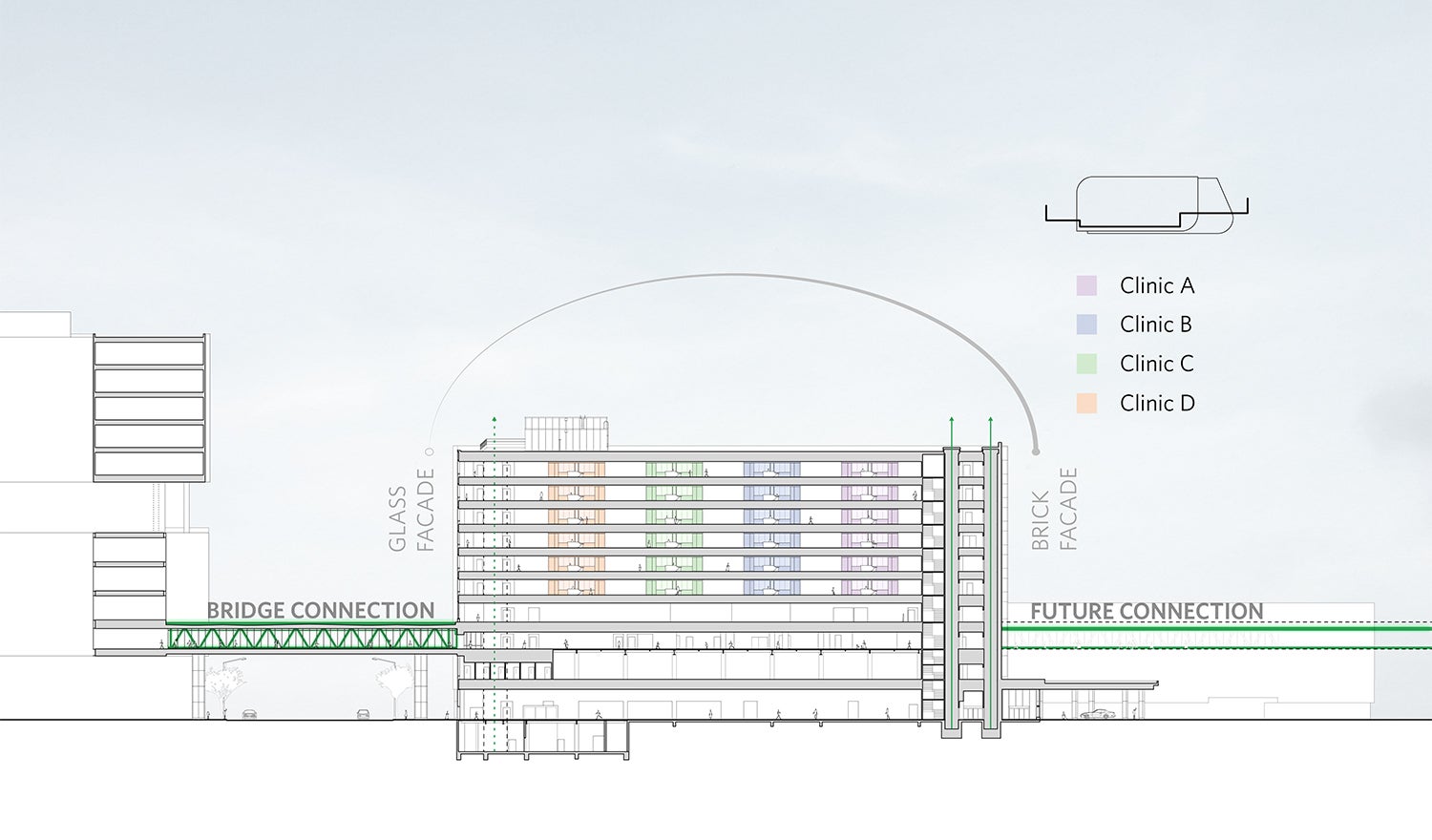
At the Rush University Medical Center Joan & Paul Rubschlager Building in Chicago, each typical clinic floor houses four identical clinical modules. Adaptability is embedded into the design, where the flexible module can support all different types of clinical services easily without reconfiguration as care models change over time. The design for the fourth level “Main Street” is being implemented as a connected design language throughout the campus.
Over-customization should be avoided. Prioritizing flexibility enables new ideas and future agility without committing to ephemeral details that drive renovations. Modular, repeated components support prefabrication, reduce construction time, and facilitate consistent quality.
Enhance the Experience to Build Trust
Patients approach health services differently. making it essential to create places of care that serve both today’s and tomorrow’s needs. While meeting general expectations, design must remain adaptable to future generations, strengthening brand identity and building patient loyalty.
The physical environment shapes both behavior and emotion. Mapping patient, visitor and staff experiences often reveals feelings of being overwhelmed upon arrival, calling for design that empowers autonomy and choice. By identifying moments of confusion or disconnection along these journeys, teams can adjust planning to better support emotional well-being. Designing these touch points relies on empathy, an essential part of the creative process.
The Moffitt Cancer Center, Moffitt McKinley Hospital in Tampa, Florida, is designed to evoke instant feelings of calm and serenity for patients, visitors, staff and caregivers as they enter the spa-like hospital environment.
The Technology Challenge: Change Is Always Around the Corner
Technology has the potential to turn medicine and healthcare delivery on its head, with rapid advancements such as artificial intelligence (AI) alongside existing tools like wearable sensors. Adoption is often slowed by valid concerns around patient confidentiality. Regardless of pace, designers and planners must recognize that healthcare delivery will continue to evolve.
At the VCU Health Adult Outpatient Center, Massey Cancer and adult outpatient multispecialty clinics share one tower with clearly separated patient and care delivery flows, giving the building multiple purposes. For both programs, technology continues to advance. Raising the linear accelerator out of the basement and above grade improves patient experience but also allows for use of the pull out façade panels for simpler future technology and equipment upgrades.
The physician-patient relationship has long defined the healthcare journey, but that paradigm is evolving. Patients now arrive informed by online sources and wearable data, opening opportunities for remote analysis by physicians or AI. Supported by video and remote communications platforms, future outpatient facilities may become smaller, distributed, and modular, consolidating costly equipment while remaining flexible to accommodate change.
Design Matters: Considering Context
Cancer centers are increasingly investing in outpatient facilities to extend their brand and create consistency across inpatient and outpatient services. These models inform the design of places that enhance the health journey, build patient loyalty and serve their communities. At the VHC Health Outpatient Center in Arlington, Virginia, the design responds to surrounding residential neighborhoods, prioritizing human scale, pedestrian experience and neighborhood enhancement.
These facilities succeed when they are rooted in community and project pride of place — welcoming to all, easy to approach, and intentionally porous in how they meet their surroundings. By softening edges between the building and the neighborhood, they become familiar destinations rather than isolated institutions. This openness supports broader outreach efforts and helps establish the center as an active participant in community health. They also function as true places for health, reinforcing the continuum of care. When outpatient environments are designed to strengthen these connections, patients and families experience care as coordinated and intuitive.